Quiz – Name that Score!
By William Aird
Clinical prediction rules are used to estimate the probability of a specific disease or its clinical outcome. Several of them have been validated in benign hematology and are used to inform clinical decision making. In this quiz, we will focus on 4 such scores. We will cover the remainder in a subsequent quiz.
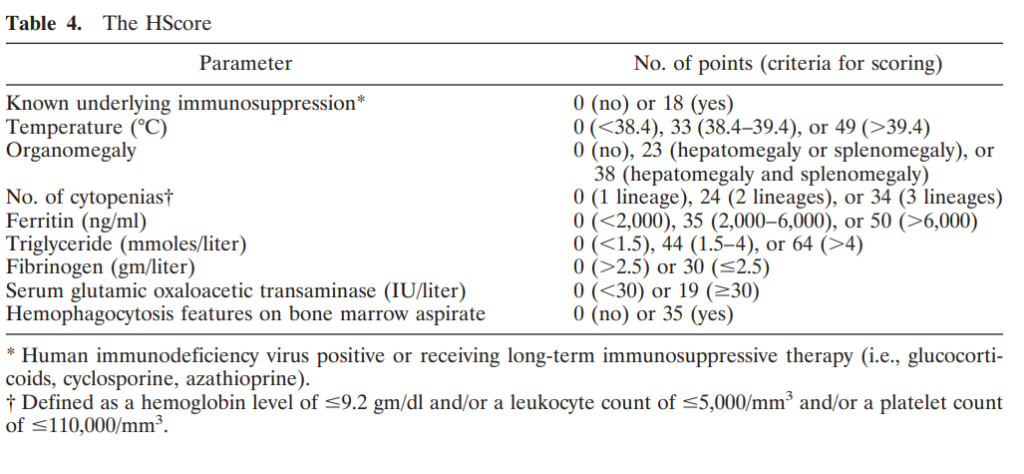
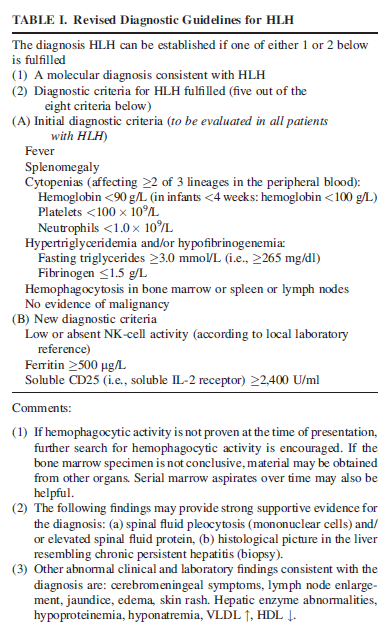
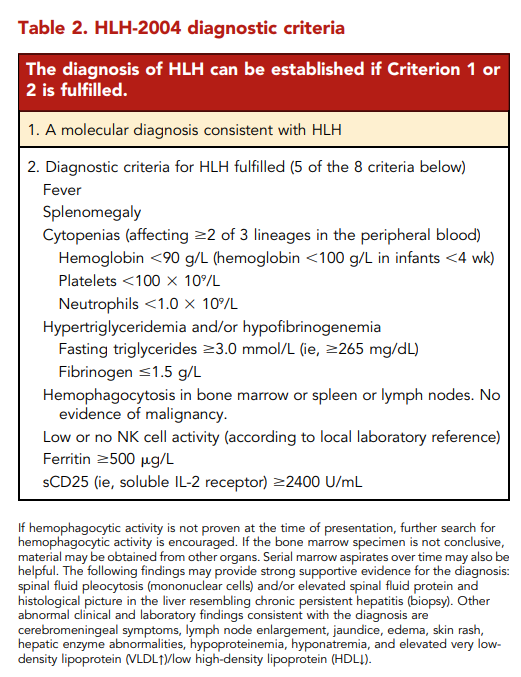
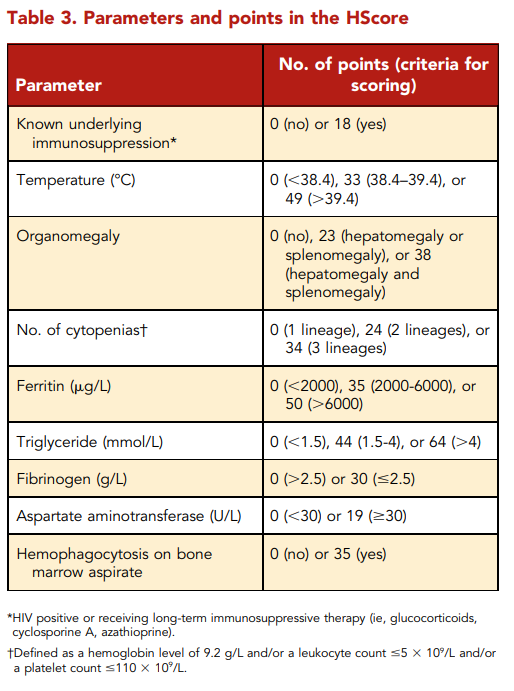
HScore is used to diagnose HLH. What other scoring system can be used for the same purpose?
So, we have two clinical scores for HLH. One is called the HScore. The other is termed the HLH-2004 diagnostic criteria.
What are some components of the HScore?
What are some differences between the HSscore and the HLH-2004 diagnostic criteria?
Comparison of HLH-2004 and HScore
| Parameter | HLH-2004 diagnostic criteria | HScore | Comments |
|---|---|---|---|
| Known underlying immunosuppression | NA | 0 (no) or 18 (yes)+ | HIV positive or receiving long‐term immunosuppressive therapy (e.g., glucocorticoids, cyclosporine) |
| Fever | 0 (<38.5) or 1 (38.5) | 0 (<38.4), 33 (38.4–39.4), or 49 (>39.4) | Persistent or recurrent high fever. Nearly universal in untreated HLH |
| Hepatomegaly | NA | 0 (no), 23 (hepatomegaly or splenomegaly), or 38 (hepatomegaly and splenomegaly | Abnormal liver tests reported in about 80% of adults with HLH (hypoalbuminemia detected in most adults with HLH) |
| Splenomegaly | 0 (no) or 1 (yes) | 0 (no), 23 (hepatomegaly or splenomegaly), or 38 (hepatomegaly and splenomegaly) | Splenomegaly may be caused by infiltration by activated lymphocytes and histiocytes or it by an underlying condition triggering HLH |
| Cytopenias | 0 (one lineage) or 1 (two or three lineages)* | 0 (one lineage), 24 (two lineages), or 34 (three lineages)** | Especially thrombocytopenia and anemia in early stages; results primarily from severe cytokine-mediated myelosuppression |
| High Ferritin level (ng/ml) | 0 (<500) or 1 (500) | 0 (<2,000), 35 (2,000-6,000), or 50 (>6,000) | No specific ferritin level determined to be specific for HLH. However, the higher the ferritin the likelier the diagnosis of HLH |
| Elevated triglyceride level | NA | 0 (<1.5), 44 (1.5-4), or 64 (>4) | hypertriglyceridemia is detected in 42%-85% of adults |
| Low Fibrinogen level | NA | 0 (>2.5) or 30 (<2.5) | hypofibrinogenemia detected in about 50% of adults with HLH |
| Elevated triglyceride level or low fibrinogen level | Triglycerides > 265 mg/dl and/or fibrinogen </= 15 mg/dL (1) | NA | |
| AST | NA | 0 (<30) or 19 (30) | LDH and bilirubin may also be increased |
| Hemophagocytosis features on bone marrow aspirate | 0 (no) or 1 (yes) | Hemophagocytosis in bone marrow 0 (no) or 1 (yes) | If the bone marrow specimen is not conclusive, material may be obtained from other organs |
| Elevated soluble IL-2 receptor (s | 1 (sIL-2R ≥ 2,400 units/mL) | NA | sIL-2R (sCD25), a marker of T cell activation; not available at most medical centers, their utility in real-time diagnosis and monitoring remains limited |
| Low or absent NK-cell activity | 1 (Yes) | NA | Not available at most medical centers; their utility in real-time diagnosis and monitoring remains limited |
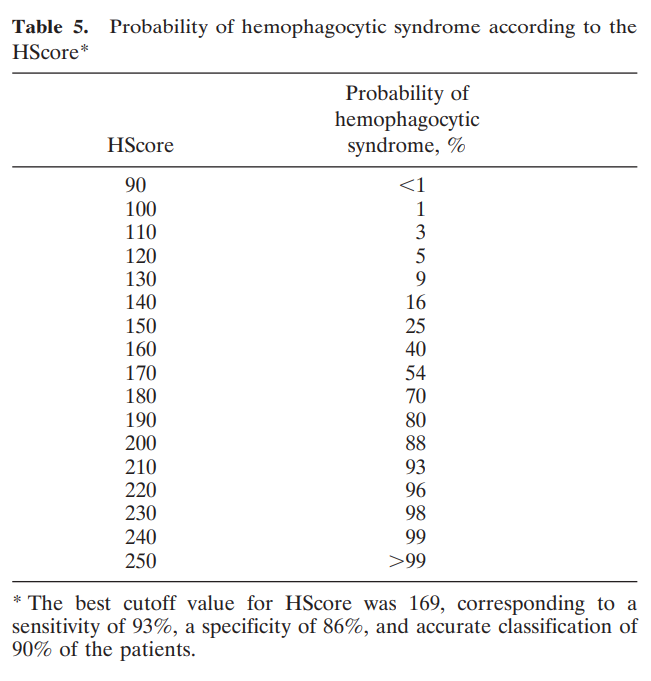
| Diagnosis | Diagnosis of HLH requires five of the above eight features | See next slide for pretest probabilities according to HScore | If hemophagocytic activity is not proven at the time of presentation, further search for hemophagocytic activity is encouraged |
Data are presented as number of points, with values in parentheses.
Other abnormal clinical and laboratory findings consistent with the diagnosis of HLH include cerebromeningeal symptoms, lymph node enlargement, jaundice, edema, skin rash, hepatic enzyme abnormalities, hypoproteinemia, hyponatremia, and elevated very low-density lipoprotein (VLDL↑)/low high-density lipoprotein (HDL↓), hyperbilirubinemia, elevated lactate dehydrogenase (LDH) and d-dimers (learn more here).
*Defined as hemoglobin less than 9.0 g/dL, platelets less than 100 x 109 /L, and neutrophils less than 1.0 x 109/L
**Defined as hemoglobin ≤9.2 g/dL (≤5.71 mmol/L) and/or WBC ≤5 x 109/L and/or platelets ≤110 x 109/L
Data from the original study reporting the HLH-2004 criteria
True or false: ferritin >500 ng/ml is specific for HLH
What are some additional differences between HScore and the HLH-2004 criteria?
What do the guidelines say about HLH-2004 and the HScore?
Recommendations for the management of HLH in adults, based on expert opinion:
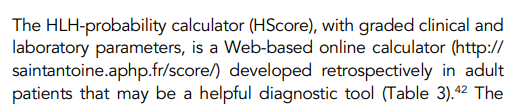
More about HLH-2004 criteria and the HScore
| Attribute | HLH-2004 | HScore |
|---|---|---|
| Original cohort | Children | Adults |
| Number of variables | 8 | 9 |
| Graded clinical and laboratory parameters | No | Yes |
| Original publication | Henter et al (children) | Fardet et al (adults) |
| Subsequent validation | Debaugnies et al (adults and children) | Debaugnies et al (adults and children) |
| Calculator | Not available | MdCalc |
Is a clinical prediction score recommended for diagnosing disseminated intravascular coagulation (DIC)?
There are three published scoring systems for DIC. Each uses similar parameters, and all are useful for diagnosing DIC and predicting poor outcome:
- ISTH – the most commonly used DIC scoring system in Europe and the US
- JAAM
- JMHLW
ISTH, International Society of Thrombosis and Haemostasis; JAAM, Japanese Association of Acute Medicine; JMHLW, Japanese Ministry Health, Labour and Welfare (JMHLW)
We will focus on the ISTH scoring system in this quiz.
What are some of the parameters used in the ISTH DIC score?
Is it important to diagnose an underlying cause of DIC for diagnostic purposes?
ISTH scoring system – Simple, just 4 parameters based on widely available, routine coagulation tests.
| Parameter | Score | Comment |
|---|---|---|
| Fibrinogen (g/L) | >1 (0) <1 (1) | Overall sensitivity of low fibrinogen level reported to be about 30% |
| Prothrombin time (PT) (seconds) | <3 (0) 3-6 (+1) >6 (+2) | Elevated in 50%-60% of patients with DIC at some point during course of illness |
| Platelet count | >100 (0) 50-100 (+1) <50 (+2) | Thrombocytopenia reported to occur in up to 98% of DIC cases |
| D-dimers or FDPs | No increase (0) Moderate increase (+2) Severe increase (+3) | Elevated FDPs and D-dimers are sensitive, but not specific for DIC |
Data are presented as values with number of points in parentheses.
A total score of ≥5 is compatible with diagnosis of DIC
To reiterate, DIC is diagnosed when the ISTH DIC score is 5 or higher:
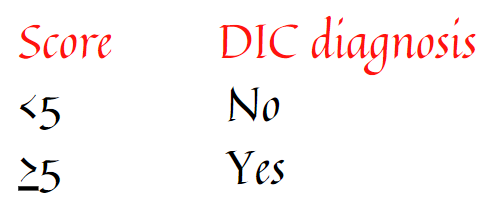
More about the ISTH DIC score
Original publication on the ISTH score can be found here.
Prospective validation study can be found here – sensitivity of the DIC score 95%, specificity 98%
See ISTH calculator
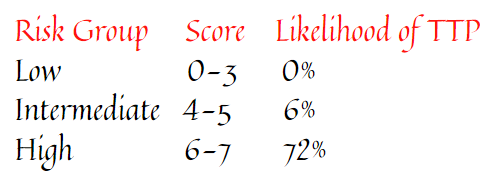
What is the PLASMIC score used for?
What are some variables in the PLASMIC score for TTP?
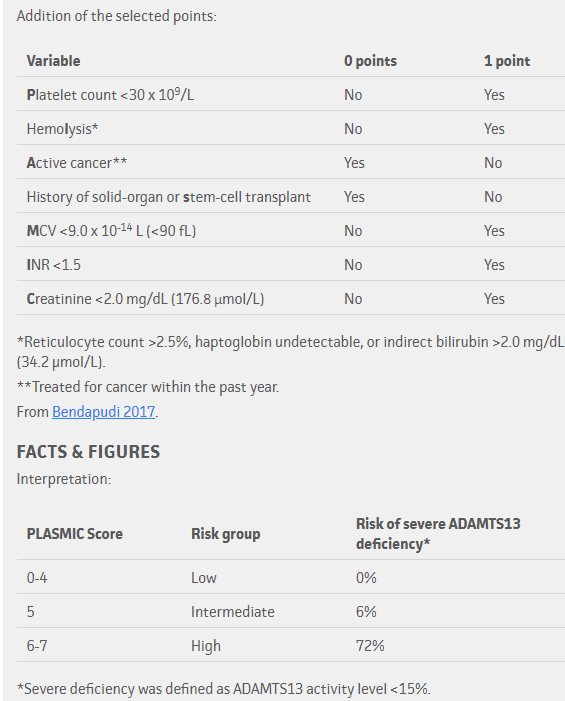
To reiterate, the pretest probability of TTP based on PLASMIC score:
What is the explanation for a low MCV (one of the PLASMIC criteria) in TTP?
Can the PLASMIC score replace the need to measure ADAMTS13 levels
How well does the PLASMIC score perform (when dichotomized at high [scores 6-7] vs. low-intermediate risk [scores 0-5])?
How well does the PLASMIC score perform (when dichotomized at high (scores 6-7) vs. low-intermediate risk (scores 0-5))?
All answers are correct – the PLASMIC score performs pretty well, especially in ruling out TTP
What do the clinical practice guidelines say?
ISTH guidelines for the diagnosis of thrombotic thrombocytopenic purpura:
“The panel agreed that any diagnostic strategy would have to start with a thoughtful assessment of the patient’s pretest probability of having TTP and the use of a formal risk assessment or pretest probability assessment model would not be inappropriate [hardly an enthusiastic endorsement for using a scoring system!]… they noted that both the PLASMIC and the French scores [details of the French score can be found here] were designed for adult populations with no comorbid conditions (eg, pregnancy, cancer, sepsis, organ/tissue transplantation, etc.), which may not be reliable in assessing children and patients with other comorbidities.”
“… in settings with a timely access to plasma ADAMTS13 activity testing and for patients with a high clinical suspicion (≥90% pretest probability) of TTP (eg, based on clinical assessment or a formal clinical risk assessment method), the panel suggests the following diagnostic strategy. (A conditional recommendation in the context of low certainty evidence)”
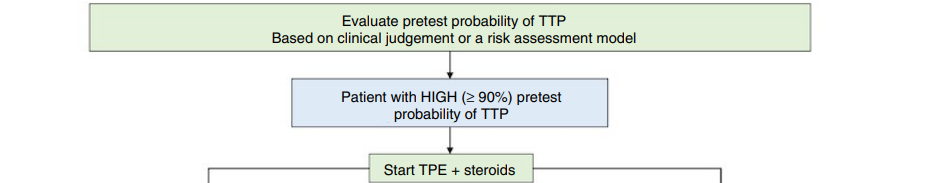
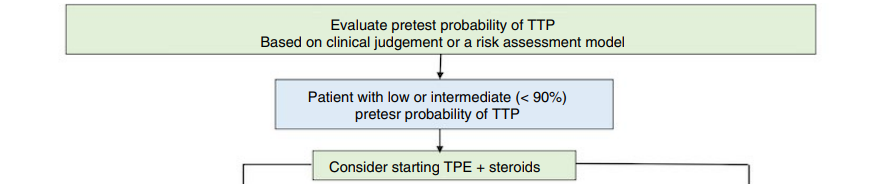
According to these practice guidelines, then, clinical judgement independent of a clinical scoring system, is sufficient for diagnosis. Importantly, the use of a clinical scoring system as the PLASMIC score, has a hugely significant impact on therapeutic decisions.
More about PLASMIC score:
See calculator
Note: the PLASMIC score was derived in adult populations with no comorbidities
What is the most commonly used score to diagnose heparin-induced thrombocytopenia (HIT)?
What are the T’s in the 4T score?
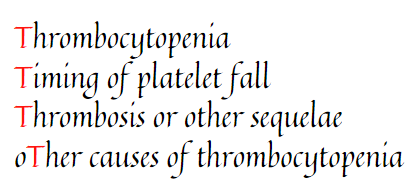
Another simple score – just 4 parameters!
| Parameter | 2 points | 1 point | 0 points | Comment |
|---|---|---|---|---|
| Thrombocytopenia | Platelet count fall > 50% AND platelet nadir ≥ 20 × 109 L−1 | Platelet count fall 30%–50% OR platelet nadir 10–19 × 109 L−1 | Platelet count fall < 30% OR platelet nadir < 10 × 109 L−1 | Fall from highest platelet count that immediately precedes the putative HIT-related platelet count fall. 95% of cases of HIT are reported to develop in temporal association with heparin therapy; typically > 50% platelet count fall, but not to levels < 20 × 10 9 /L; only a few patients show 30%-50% platelet count fall; typical nadir is 40-80 × 109/L, with median of 55 × 109/L |
| Timing of platelet count fall | Clear onset between days 5 and 10 OR platelet fall ≤ 1 day (prior heparin exposure within 30 days) | Consistent with days 5–10 fall, but not clear (e.g. missing platelet counts) OR onset after day 10 OR fall ≤ 1 day (prior heparin exposure 30–100 days ago) | Platelet count fall < 4 days without recent heparin exposure | Day 5 to 10 for initial platelet count fall with day 0 representing first heparin exposure; earlier fall if patient exposed to heparin with previous 30 days. Days are rounded off. For example, day 4.3 would count as day 4. |
| Thrombosis or other sequelae | New thrombosis (confirmed) OR skin necrosis at heparin injection sites OR acute systemic reaction after intravenous heparin bolus | Progressive or recurrent thrombosis or nonnecrotizing (erythematous) skin lesions or suspected thrombosis (not proven | None | |
| Other causes for thrombocytopenia | None apparent | Possible | Definite |
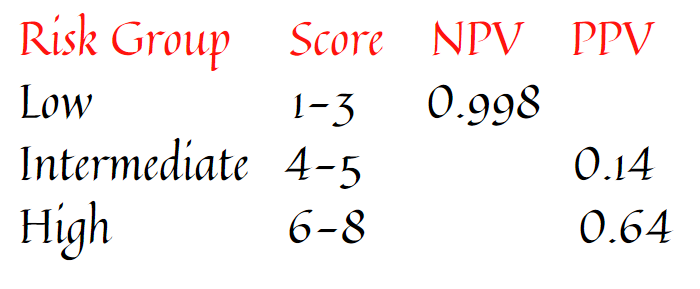
Scoring 0, 1, or 2 points for each of 4 categories, maximum possible score = 8 Low score (0-3 points), intermediate score (4 or 5 points), high score (6-8 points).
- Low score 0-3 points
- Intermediate score 4-5 points
- High score 6-8 points
Low 4Ts score may rule out HIT but high 4Ts score may not be sufficient to diagnose HIT.
The negative and positive predictive values of the 4T score based on points:
Why are the PT, aPTT or fibrinogen not part of the 4T score?
How often should the HIT score be calculated?
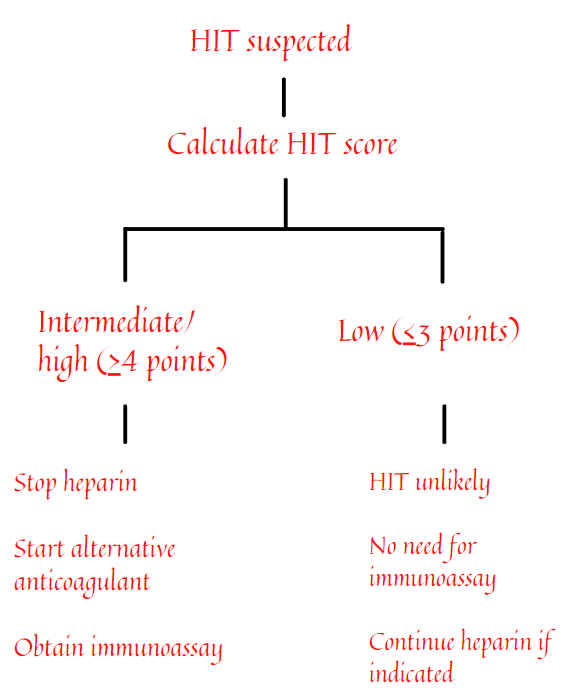
How can the 4T score be used to inform diagnosis/therapy of HIT?
Incorporating the 4T score into a diagnostic and therapeutic algorithm
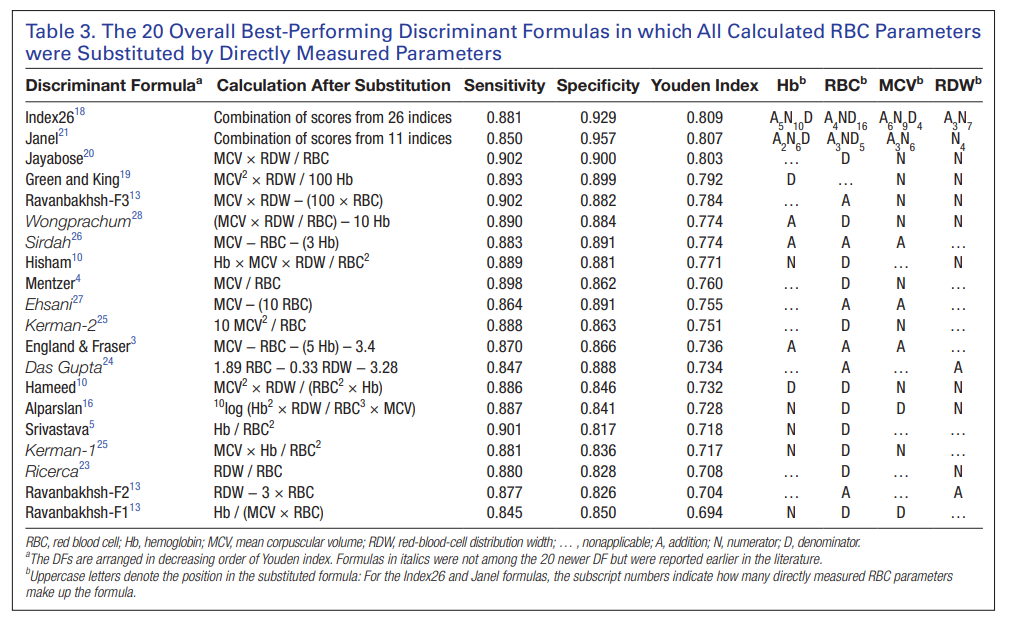
What is the Mentzer index used for?
What are the variables is the Mentzer index?
The Mentzer index:

Ratio > 13 suggests iron deficiency anemia; ratio < 13 suggests thalassemia trait
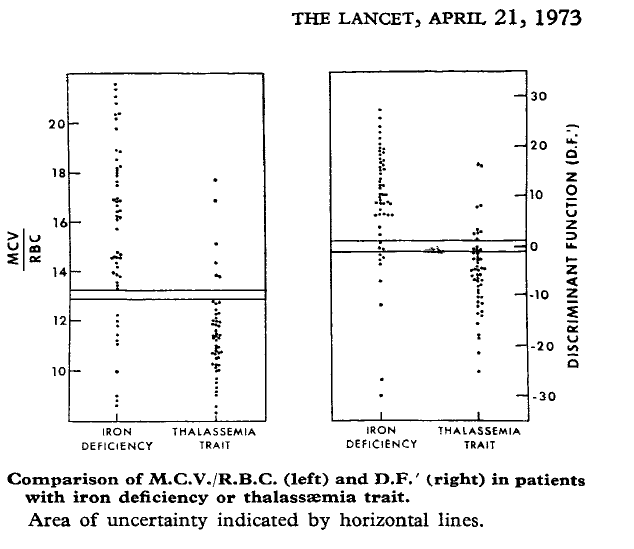
The Mentzer index is just one of many formulas reported to help distinguish between iron deficiency anemia and thalassemia minor!
True of false: Like the DIC score or the HScore, the Mentzer index is necessary to make a diagnosis for conditions that lack a diagnostic test?
Summary
We have covered four clinical prediction rules in this quiz. The purpose of this exercise was to familiarize yourself with the various systems, to recognize that alternative prediction rules often exist for a given disease entity, and to appreciate the vital importance of such scores – limitations and all – in directing therapeutic decisions, often in cases with life and death consequences. We will over additional clinical prediction scores in subsequent quizzes.