Postscript
Prev
1 / 0 Next
Prev
1 / 0 Next
Introduction
- Polyclonal gammopathy:
- Is a type of hypergammaglobulinemia that results from an increased production of several different immunoglobulins by plasma cells.
- Is most commonly associated with liver disease, acute or chronic inflammation, autoimmune disorders and certain malignancies.
- Is generally considered a benign condition that does not progress to overt malignancy.
- May provide an important clue for less common difficult-to-diagnose conditions, such as eosinophilic granulomatosis with polyangiitis, IgG4-related disease, and Rosai–Dorfman disease.
- Is part of the diagnostic criteria for rare diseases such as:
- Idiopathic multicentric Castleman disease:
- Polyclonal hypergammaglobulinemia (total gamma globulin or immunoglobulin G >1700 mg/dL) is one of 11 minor criteria.1
- Autoimmune lymphoproliferative syndrome (APLS):
- Autoimmune cytopenias (hemolytic anemia, thrombocytopenia, or neutropenia) AND elevated immunoglobulin G levels (polyclonal hypergammaglobulinemia) is part of the revised diagnostic criteria for APLS.2
- Idiopathic multicentric Castleman disease:
- Although clinical practice guidelines exist for approaching a patient with a monoclonal paraprotein, there is no such guidance for working up an individual with polyclonal hypergammaglobulinemia.
Definitions
- Hypergammaglobulinemia:
- Results from overproduction of immunoglobulins by plasma cells detected on serum protein electrophoresis (SPEP).
- Classified as:
- Polyclonal – generalized increase in immunoglobulins associated with the diffuse activation of B cells, plasma cells or lymphoplasmacytic cells.
- Monoclonal – associated with excessive production of immunoglobulins from a single clone of plasma cells or lymphoplasmacytic cells.
- Polyclonal gammopathy is usually defined as gamma-globulin level above the threshold applying to healthy blood donors:
- No consensus threshold for gamma-globulin level.
- Threshold historically defined as >30 g/L, more recently redefined as >19 g/L.
Causes
- Causes of polyclonal gammopathy include:
- Infectious disease:
- Viral:
- HIV
- Chronic cytomegalovirus (CMV) infection
- Chronic Epstein Barr virus (EBV) infection
- Varicella zoster
- Bacterial:
- Bacterial endocarditis
- Whipple disease
- Mycobacterial:
- Mycobacterium tuberculosis
- Mycobacterium leprae
- Parasitic:
- Toxoplasmosis
- Visceral Leishmaniosis
- Fungal:
- Invasive Aspergillosis
- Viral:
- Autoimmune diseases:
- Sjogren’s disease
- Rheumatoid arthritis
- Systemic lupus erythematosus (SLE)
- Scleroderma
- Dermatomyositis and polymyositis
- Vasculitis:
- Anti-neutrophil cytoplasmic autoantibody (ANCA) vasculitis:
- eosinophilic granulomatosis with polyangiitis (EGPA)
- granulomatosis with polyangiitis (GPA)
- microscopic polyangiitis (MPA)
- Giant cell arteritis
- Anti-neutrophil cytoplasmic autoantibody (ANCA) vasculitis:
- Graves’ disease
- IgG4-related disease
- Hematologic:
- Autoimmune cytopenias
- Autoimmune lymphoproliferative syndrome (ALPS)
- Castleman’s disease
- Rosai–Dorfman disease
- Hypereosinophilic syndromes
- Hemophilia A
- Hemoglobinopathies
- Hematologic malignancies:
- B cell lymphoproliferative disease
- T-cell lymphoma
- Large granular lymphocyte (LGL) leukemia
- Angioimmunoblastic lymphadenopathy
- Solid tumor malignancy
- Sarcoidosis
- Gaucher’s disease
- Inflammatory bowel disease:
- Crohn’s disease
- Ulcerative colitis
- Liver diseases – the most common cause of polyclonal hypergammaglobulinemia in the primary care setting:
- Autoimmune hepatitis
- Viral hepatitis
- Alcoholic and non-alcoholic steatohepatitis
- Alcoholic cirrhosis
- Primary biliary cirrhosis
- α1-Antitrypsin deficiency
- Infectious disease:
- Causes of polyclonal gammopathy according to isotype:3
- Polyclonal increases in IgG concentration:
- Liver disease
- Autoimmune and autoinflammatory disease
- Vasculitis; infection
- Hematological disorders
- Non-hematological malignancy
- Immunodeficiency
- IgG4-related disease
- Iatrogenic (from intravenous immunoglobulin administration)
- Polyclonal increases in IgM concentration:
- Impaired B-cell immunoglobulin class switching
- Acute infection
- Hyper-IgM syndrome
- Polyclonal increases in IgA concentration:
- Liver disease
- Alcohol excess
- IgA vasculitis (eg, Henoch–Schönlein purpura)
- HIV infection
- Autoimmune disease:
- Celiac disease
- Rheumatoid arthritis
- Systemic lupus erythematosus
- IgA nephropathy
- Polyclonal increases in IgD concentration:
- Hyper-IgD syndrome (commonly caused by MVK mutations; also presents with elevated IgA concentrations)
- Polyclonal increases in IgE concentration:
- Allergy
- Atopy
- Asthma
- Lymphoma
- Hyper-IgE syndrome (commonly caused by STAT3 mutations)
- Polyclonal increases in IgG concentration:
- Causes according to CRP level:
- Persistently high C-reactive protein concentrations (≥30 mg/L):
- Chronic infection
- Malignancy
- Hematological disorders:
- Multicentric Castleman disease
- Rosai–Dorfman disease
- Autoimmune and autoinflammatory diseases:
- Vasculitis:
- Dermatomyositis and polymyositis
- Inflammatory bowel disease
- Ankylosing spondylitis
- Familial Mediterranean fever
- Sarcoidosis
- Vasculitis:
- Variable C-reactive protein concentrations:
- Hematological disorders:
- Lymphoma and lymphoproliferative disorders
- Autoimmune and autoinflammatory diseases:
- Sjogren’s syndrome
- Systemic lupus erythematous
- Inflammatory arthritis
- Sarcoidosis
- Hematological disorders:
- Low or modestly elevated C-reactive protein concentrations (<30 mg/L):
- Liver disease
- Hematological disorders:
- Angioimmunoblastic T-cell lymphoma
- Fanconi anaemia
- Hypereosinophilic syndromes
- Autoimmune cytopenias
- Myelodysplastic syndromes
- Hemophilia A (inherited and acquired)
- Hemoglobinopathies
- Autoimmune and inflammatory disorders:
- Graves’ disease
- Scleroderma
- Immunodeficiency syndromes
- IgG4-related disease
- Persistently high C-reactive protein concentrations (≥30 mg/L):
- Causes reported in cohort studies:
- Retrospective study of 148 patients with polyclonal hypergammaglobulinemia >30 g/L:
- Liver disease (53%)
- Autoimmune hepatitis (most common)
- Viral hepatitis
- Primary biliary cirrhosis
- Primary sclerosing cholangitis
- Ethanol-related liver disease
- Connective tissue disease (27%)
- Sjogren’s disease (most common)
- Rheumatoid arthritis
- Systemic lupus erythematosus
- Chronic infection (6%)
- HIV
- Hepatitis B
- Hepatitis C
- Bronchiectasis with chronic pulmonary infections
- Pyelonephritis
- Pulmonary tuberculosis
- Subacute bacterial endocarditis
- Hematologic disorder (5%)
- Benign lymphoproliferative disorders
- Low-grade lymphomas
- High-grade T-cell lymphoma
- Large granular lymphocytic leukemia
- Chronic myelomonocytic leukemia
- Non-hematological malignancy (6%)
- Hepatocellular carcinoma
- Ovarian carcinoma
- Squamous cell carcinoma of the lung
- Pancreatic adenocarcinoma
- Renal cell carcinoma
- Chondrosarcoma
- Liver disease (53%)
- Retrospective study of 42 patients with polyclonal hypergammaglobulinemia >100 g/L:
- HIV infection
- Chronic hepatopathy
- Sjogren’s syndrome
- Chronic kidney disease
- Sepsis
- Lymphoma
- Chronic lymphocytic leukemia
- Retrospective study of 66 patients with polyclonal hypergammaglobulinemia >20 g/L:
- Autoimmune diseases (32%):
- Sjögren syndrome
- Autoimmune vasculitis
- Systemic lupus erythematosus
- Polymyalgia rheumatica
- Rheumatoid arthritis
- Inflammatory arthritis
- Orbital inflammatory syndrome
- Adult onset Still disease
- Eosinophilic granulomatosis with polyangiitis
- Undifferentiated connective tissue disease
- Hematologic conditions (21%):
- T-cell large granular lymphocytic leukemia
- MonoMAC syndrome (GATA2 deficiency)
- Rosai-Dorfman-Destombes disease
- Polycythemia vera
- Cutaneous plasmacytosis
- Chronic lymphocytic leukemia
- Valvular hemolysis
- Iron-deficiency anemia
- Autoimmune neutropenia
- Chronic myelogenous leukemia
- Anemia secondary to occult gastrointestinal bleeding
- Hepatosplenic T-cell lymphoma
- IgG4-RD (20%)
- Liver disease (11%)
- Malignancy (2%)
- Autoimmune diseases (32%):
- Scoping review of literature reported that polyclonal hypergammaglobulinemia is associated with 115 etiologies organized into 15 nosology groups.
- Retrospective study of 148 patients with polyclonal hypergammaglobulinemia >30 g/L:
Mechanisms
- Polyclonal hypergammaglobulinemia results from chronic polyclonal stimulation of B lymphocytes.
- Precise cascade of interactions triggering polyclonal B-cell activation is still unknown. Mechanisms may include:
- Cytokine stimulation, especially interleukin-6, which is:
- A pleiotropic cytokine.
- Involved in:
- Induction of B-cell maturation into antibody-secreting cells.
- Maintenance and survival of plasma cells.
- Synthesis of acute phase proteins in hepatocytes.
- Implicated in the pathogenesis of polyclonal hypergammaglobulinemia associated with:
- Castleman disease
- Rosai–Dorfman disease
- Autoimmune hepatitis
- Chronic antigenic stimulation
- Defects in various subsets of T cells
- Cytokine stimulation, especially interleukin-6, which is:
- In cirrhosis, the loss of hepatic filtering capacity allows enteric antigens and endotoxins access to the immune system, leading to increased IgA and IgG production.
Diagnosis
- History and physical exam:
- Focus on eight causes (“buckets”) of polyclonal hypergammaglobulinemia:
- Liver disease
- Autoimmune disease and vasculitis
- Infection and inflammation
- IgG4-related disease
- Hematological disorders
- Non-hematological malignancy
- Immunodeficiency
- Iatrogenic
- Symptoms and signs:
- Secondary to the elevated immunoglobulins:
- Signs and symptoms of hyperviscosity (rare in polyclonal hyperglobulinemia, but may occur when total IgG concentration >60 g/L), including:
- Altered level of consciousness
- Visual disturbances
- High-output heart failure
- Mucosal bleeding
- Retinal hemorrhages
- Papilledema
- Signs and symptoms of hyperviscosity (rare in polyclonal hyperglobulinemia, but may occur when total IgG concentration >60 g/L), including:
- Secondary to conditions that cause the elevated immunoglobulins:
- Arthritis
- Skin lesions
- Fever and infection
- Travel and exposures
- Intravenous immunoglobulin therapy
- Family history of immunodeficiency
- Swelling of lacrimal, salivary, and parotid glands
- Lymphadenopathy
- Hepatosplenomegaly
- Signs of chronic liver disease
- Secondary to the elevated immunoglobulins:
- Focus on eight causes (“buckets”) of polyclonal hypergammaglobulinemia:
- Labs:
- Diagnosed by serum protein electrophoresis and immunofixation electrophoresis (SPEP/IFE) showing a polyclonal increase in immunoglobulins (having 1 or more heavy-chain classes and both kappa and lambda light-chain types).
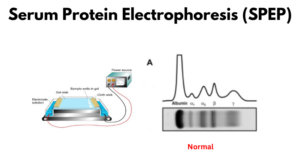
- Serum protein electrophoresis (SPEP):
- General information:
- SPEP is a method of separating proteins based on their charge.
- Serum is placed on a specific medium, and a charge is applied for a predetermined time.
- The separated proteins are transferred to special paper, which is then removed, dried, placed on a fixative to prevent further diffusion of specimen components, and then stained to visualize various protein bands.
- Coomassie brilliant blue is a common staining agent to visualize bands in SPEP.
- A densitometer is then used to quantify each fraction.
- The serum protein components are separated into five major fractions:
- Albumin – Albumin, the largest peak, lies closest to the positive electrode.
- represents the largest protein component of human serum
- Alpha-1 globulins (alpha-1 zone)
- Alpha-2 globulins (alpha-2 zone)
- Beta globulins
- Gamma globulins (gamma zone)
- Albumin – Albumin, the largest peak, lies closest to the positive electrode.
- SPEP is a method of separating proteins based on their charge.
- General information:
-
-
- SPEP in polyclonal gammopathy:
- Produces a broad band or a broad-based peak that is limited to the gamma region.
- IgG isotype is the most commonly involved immunoglobulin, followed by IgA and IgM.
- SPEP in polyclonal gammopathy:
-
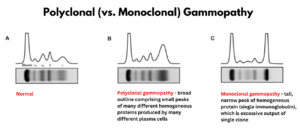
Electrophoretic patterns. A, Normal. B, Polyclonal, broad outline comprising small peaks of many different homogeneous proteins produced by many different plasma cells. C, Monoclonal, tall, narrow peak of homogeneous protein (single immunoglobulin), which is excessive output of single clone. Source.
-
-
-
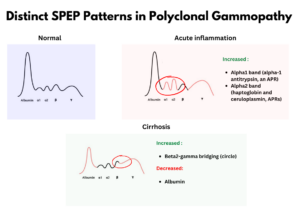
- The pattern of other bands outside the gamma zone may provide clues about the cause of polyclonal gammopathy . For example:
- Polyclonal gammopathy associated with inflammation:
- Polyclonal hypergammaglobulinemia (gamma zone)
- Increased intensity of alpha-1 and alpha-2 bands:
- Alpha-1 band – contains alpha-1-antitrypsin, which is an acute-phase reactant
- Alpha-2 band – contains haptoglobin and ceruloplasmin, which are acute-phase reactants
- Decreased intensity of:
- Albumin band (negative acute phase reactant)
- Beta-1 band (contains transferrin, a negative acute phase reactant)
- Polyclonal gammopathy associated with liver disease:
- Polyclonal hypergammaglobulinemia (gamma zone)
- Low albumin band
- Prominent beta-2 band, which leads to beta–gamma bridging:
- Abnormal protein band between the beta and gamma globulins causing lack of demarcation (loss of valley) between the the 2 peaks.
- Caused by increase in the beta and gamma regions.
- Polyclonal gammopathy associated with inflammation:
- The pattern of other bands outside the gamma zone may provide clues about the cause of polyclonal gammopathy . For example:
-
-
-
- Free light chain (FLC) assay:
- Polyclonal free light chain overproduction can occur in the setting of polyclonal gammopathy.
- Levels often correlate with:
- Other markers of B cell activation, such as total gammaglobulin and IgG levels.
- Disease activity in certain inflammatory conditions, such as rheumatoid arthritis and SLE.
- While absolute FLC levels may be elevated, the free light chain lambda: kappa ratio is normal.
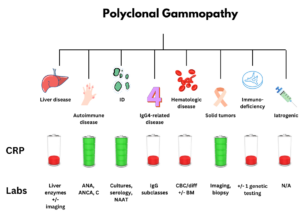
- Standard order set in a patient with polyclonal gammopathy:
- Complete blood count, white blood cell differential, and peripheral smear
- SPEP, UPEP, and quantitative immunoglobulins
- IgG subclasses
- C-reactive protein (CRP)
- Liver enzymes (AST, ALT, and ALP)
- ANA, ANCA, complement C3, complement C4, and DAT
- Hepatitis B virus, hepatitis C virus, and HIV serologies, +/– Epstein–Barr virus and human herpesvirus-8 serologies
- +/– Imaging for liver disease, lymphadenopathy, and malignancy
- +/– Bone marrow biopsy if lymphoma or hematological disorder suspected
- +/– Genetic testing for immunodeficiency syndromes
- Additional tests to consider in liver disease:
- Serologies for autoimmune hepatitis (eg, antinuclear antibodies, anti-smooth muscle antibodies, and anti-liver-kidney microsomal antibodies)
- Abdominal imaging (ultrasonography or CT)
- Ultrasound elastography (FibroScan)
- Additional tests to consider in autoimmune disease and vasculitis:
- Antinuclear antibody test, followed by more specific anti-extractable nuclear antigen
- Anti-neutrophil cytoplasmic antibodies
- Polyclonal gammopathy may result in:
- Pseudo-hyponatremia
- Decreased anion gap
- Pseudohyperphosphatemia
- Retrospective study of 148 patients with polyclonal hypergammaglobulinemia > 30 g/L:
- No significant correlation between the serum gamma globulin level and:
- Albumin
- ESR
- No significant correlation between the serum gamma globulin level and:
- Free light chain (FLC) assay:
Treatment
- Treat underlying condition; typically leads to the resolution of hypergammaglobulinemia (polyclonal gammopathy.
- No specific therapy for hypergammaglobulinemia (polyclonal gammopathy).
- In rare cases in which polyclonal hyperglobulinemia results in hyperviscosity, no pharmacologic technique has been shown to consistently and rapidly reduce the immunoglobulin levels. In this circumstance, plasma exchange would be recommended.4
Prev
1 / 0 Next
