Treatment

What are the major principles of disseminated intravascular coagulation (DIC) treatment?

To understand the challenge of treating disseminated intravascular coagulation (DIC), consider the following bonfire analogy. Assume you are camping in sub-zero temperatures at night and the heat from the fire you have built is your only way to survive the frigid temperature. There is more than enough wood around to keep the fire going. But there is catch: the black smoke arising from the fire is toxic and will lead to your demise if excessive. So, you must add just enough wood to maintain the fire without creating too much smoke.
In DIC, the clotting cascade is consumed, just as firewood is burned, and in doing so it creates fibrin, which occludes small vessels, just as the black smoke destroys the lungs. We are much better at detecting factor consumption (depletion of firewood) than we are the microvascular occlusion (the black smoke). An elevated PT, low fibrinogen, increased D-dimers/FDPs and decreased platelet count are all markers of consumption. So too is bleeding. In contrast, organ dysfunction, for example, skin necrosis, renal failure and cardiac ischemia may be subtle in its presentation and may have multiple causes. It may represent microvascular clot formation (though such thrombi are difficult to detect even at autopsy), or it may reflect other contributing factors, such as hypotension with secondary hypoperfusion or the effect of drugs. As a result, our natural tendency is to treat patients with DIC by replacing the missing factors, while ignoring the fibrin that is accumulating in the body. So, we are throwing fuel to the fire, when what we really need is a balance between replacement of factors and inhibition of thrombin generation and fibrin deposition.
A reminder of this patient’s hematological parameters at time of admission:
| Parameter | Result |
|---|---|
| Hemoglobin (Hb) | 10.6 g/dL |
| Platelets | 10 x 109/L |
| Prothrombin time (PT) | 18.4 seconds |
| Fibrinogen | 133 mg/dL |
What would you like to recommend to the team taking care of the patient?









Replacement therapies include:
- Platelet transfusions
- Fresh frozen plasma
- Cryoprecipitate
- Others:
- Prothrombin complex concentrate
- Fibrinogen concentrate
Replacement therapies include:
| Product | Indication |
|---|---|
| Platelet transfusions | Recommended in patients with active bleeding plus platelet count < 50 × 109/L, or high risk of bleeding owing to platelets < 20 × 109/L. |
| Fresh frozen plasma (FFP) | Recommended in patients with active bleeding or requiring an invasive procedure and either prolonged PT/aPTT (> 1.5 × normal) or decreased fibrinogen (< 1.5 g/L). |
| Cryoprecipitate | Recommended for patients with active bleeding plus severe hypofibrinogenemia (< 1.5 g/L) that persists despite FFP replacement. |
| Prothrombin complex concentrate (PCC) | May be considered in actively bleeding patients if FFP transfusion is not possible. |
Inhibitory therapies include:
- Therapeutic doses of heparin
- Anticoagulant factor concentrates:
- Activated protein C
- Antithrombin
- Recombinant thrombomodulin



Inhibitory therapies include:
| Product | Indication |
|---|---|
| Heparin (therapeutic) | May be considered in cases where thrombosis predominates; LMWH recommended over UFH. |
| Antithrombin | No formal recommendation due to lack of evidence of benefit, but may be considered. |
| Recombinant thrombomodulin | No formal recommendation due to lack of evidence of benefit, but may be considered. |
| Protein C | Has been used in patients with purpura fulminans. |
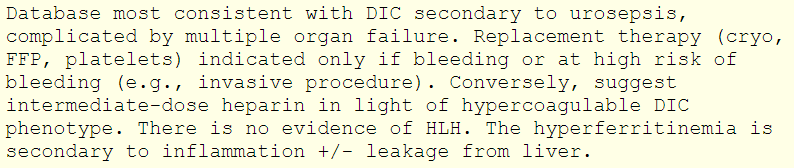
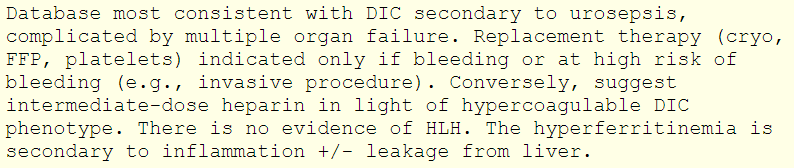
Let’s return to the patient. Here is an excerpt of the recommendations from the hematology consult service: