Treatment

To summarize at this point, we have a 72 year-old woman with an extremely elevated Hct (polycythemia) who presents with gouty arthritis of her left elbow, and possible symptoms of hyperviscosity (fatigue, “brain fog”). There are no obvious causes of secondary polycythemia, and her complete blood count and differential show concomitant leukocytosis and thrombocytosis, with basophilia – all consistent with a diagnosis of polycythemia vera.
The erythropoietin level eventually returned low, and most importantly the Jak2 V617F mutation ultimately returned positive, securing the diagnosis.
What are treatment options for reducing the Hct?
There are three cornerstones to treating polycythemia vera. All of them aim to reduce the incidence of thrombotic complications. They do not cure the disease or alter the risk of transformation to acute leukemia:
- Phlebotomy
- Cytoreductive therapy
- Anti-platelet agents
Let’s consider each in turn.
Phlebotomy:
- Currently considered standard of care for treatment of patients with polycythemia vera (PV).
- Can be used as:
- Emergency therapy for patients with high probability of having PV presenting with very high hematocrit and clinical signs of hyperviscosity – one protocol is to remove 300-400 mL of blood every other day or twice per week until target hematocrit is achieved.
- Long-term maintenance therapy.
- Goal is to maintain hematocrit < 45%.
- Reported to improve overall and thrombosis-free survival.
NOTE: Red blood cell apheresis is an alternative to phlebotomy in cases of severe vascular complications when rapid attainment of target hematocrit is required or prior to emergency surgery in patients with extremely high hematocrit value to decrease risk of perioperative vascular complications.
Cytoreductive therapy:
- First line therapy in high risk patients (> 60 years old and/or history of vascular event).
- Options include:
- Hydroxyurea:
- Antimetabolite that prevents DNA synthesis by inhibiting ribonucleoside reductase.
- Suggested starting dose 15-20 mg/kg daily until response is obtained, then maintain complete blood count within normal range with lowest possible dose.
- Interferon-alfa
- Ruxolitinib
- Hydroxyurea:
Antiplatelet agents:
- Low-dose aspirin (81 mg daily) recommended for management of polycythemia vera (PV) unless contraindicated.
- Contraindicated in patients with clinically significant acquired von Willebrand syndrome (AVWS):
- Screen all patients with PV and platelet count > 1,000 × 109/L for AVWS.
- Consider withholding aspirin if ristocetin cofactor activity < 20%.
The patient was treated with daily phlebotomy. The response in hemoglobin (Hb) and hematocrit (Hct) is shown below:
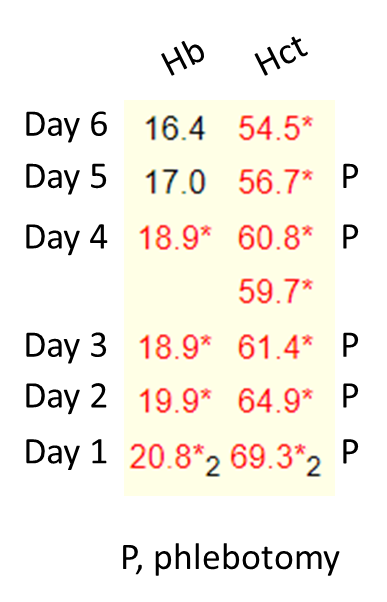
She was also started on low dose aspirin. However, hydroxyurea was not started until the Jak2 mutation status returned positive.

