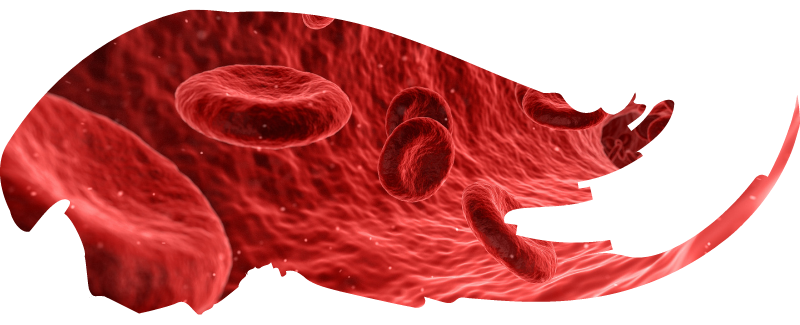
About Iron Deficiency Anemia

Description/definition:
Iron deficiency anemia may be defined as anemia caused by absent iron stores.





Pathophysiology:
Iron deficiency anemia occurs when iron output (almost always in the form of blood loss) outpaces iron intake (which can be affected in malabsorption states). It may also occur in cases of increased iron demand, for example in multiparous women.





Diagnosis:
The history, physical exam and CBC give important clues to the diagnosis of iron deficiency anemia. The serum iron may be low and the TIBC elevated, leading to a low transferrin saturation. The diagnosis is confirmed by a low serum ferritin level. Diagnostic difficulties may arise when the ferritin is increased on account of inflammation, ferritin leak (for example, in acute liver failure) and congenital hyperferritinemia (in which case ferritin gene expression is marching to its own tune, oblivious to iron stores in the body).





Treatment:
Treatment includes iron supplementation, either by the oral route or the intravenous route. When giving oral iron, there is an increasing trend to administer just one pill a day (for example, ferrous gluconate 325 mg) or every other day for 3-6 months. An advantage of IV iron is that it can replenish iron stores with just one or two injections, it bypasses issues with iron malabsorption, and it negates the need for months of oral iron, which is often poorly tolerated. These advantages must be weighed against risk of developing a reaction to IV iron. The use of oral vs. IV iron requires shared decision making.





