Treatment

Overview
- Acute chest syndrome (ACS) can be a severe life-threatening condition.
- Patients with ACS should be hospitalized.
- Early recognition of progression to acute respiratory failure is vital.
- ACS can be severe in all sickle genotypes, with similar death rates per event in HbSS and HbSC.
- Patients should be treated aggressively irrespective of their sickle genotype.
- Even with good medical treatment, overall mortality rates of up to 3% are reported, with the overall death rate in adults being four times higher than in children.
The immediate aim of treatment in acute chest syndrome (ACS) is to prevent or reverse acute respiratory failure. The key to success is early recognition of ACS and institution of treatment without delay.
Which of the following is/are used to treat patients with acute chest syndrome?
Treatment of acute chest syndrome (ACS) includes:
- Oxygen – to maintain arterial oxygen saturation of greater > 95%.

- Intravenous fluids – if patient cannot take adequate fluids by mouth.

- Pain relief:
- All patients with ACS should be given prompt and adequate pain relief.
- Care must be taken to avoid alveolar hypoventilation from opioid overdose.

- Incentive spirometry while awake:
- Should be also considered in all patients with ACS.
- Has proven benefit in preventing ACS in patients with chest or rib pain.

- Antibiotics – should be used even if blood cultures and sputum cultures are negative.
- Advanced respiratory support as needed
- Transfusion (see next slide)
Red cell transfusion
There are two types of blood transfusion:

Not all patients with ACS will require a blood transfusion.
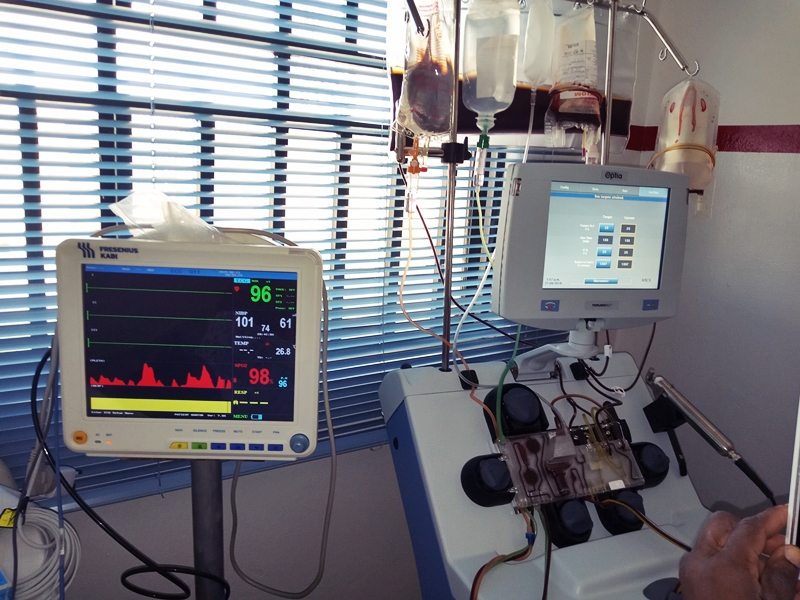
Automated red cell exchange (RCE) (also called erythrocytapheresis):
- Involves removal of the patient’s red cells and replacement with cells from the donor.
- May be automated or manual.
- Requires apheresis machines and operators with technical expertise and may only be available at specialty centers.
- Typically replaces one or two times the patient’s total red cell volume, more than used in simple transfusion.
- Despite increased exposure to donors with RCE compared to simple transfusion, several studies have shown no increase in alloimmunization rates associated with RCE.
- Red cell replacement volume and hematocrit can be tightly controlled with RCE, allowing for significant reductions in HbS levels, while minimizing or preventing iron loading.
The following are recommendations from three guideline organizations:
National Heart, Lung, and Blood Institute (NHLBI):
- In people with sickle cell anemia (SCA), give simple blood transfusion (10 mL/kg red blood cells) to improve oxygen carrying capacity to people with symptomatic acute chest syndrome (ACS) whose hemoglobin concentration is >1.0 g/dL below baseline. If baseline hemoglobin is 9 g/dL or higher, simple blood transfusion may not be required.
- In all persons with sickle cell disease (SCD), perform urgent exchange transfusion—with consultation from hematology, critical care, and/or apheresis specialists—when there is rapid progression of ACS as manifested by one of more of the following:
- Oxygen saturation below 90 percent despite supplemental oxygen.
- Increasing respiratory distress.
- Progressive pulmonary infiltrates.
- Decline in hemoglobin concentration despite simple transfusion.
British Committee for Standards in Haematology (BCSH):
- A simple (‘top-up’) transfusion:
- Should be considered in patients with a PaO2 of less than 90 kPa on room air, but may also be needed at less severe degrees of hypoxemia, depending on the individual patient’s history and clinical features, or if the patient’s oxygen requirements are increasing.
- Aiming for a final hemoglobin concentration of 10–11 g/dL, is often effective at preventing progression.
- An exchange transfusion:
- Indicated for patients:
- Who show features of severe disease.
- In those who deteriorate despite an initial simple transfusion.
- In those with a higher hemoglobin concentration (>9.0 g/dL).
- With exchange transfusion the final hemoglobin target should also be 110–110 g/l but a lower HbS% will be achieved.
- There is no evidence for an optimal HbS% target post-exchange transfusion. In practice a target of < 30– 40% is often used, but clinicians should be guided by the clinical response.
- Indicated for patients:
American Society of Hematology (ASH):
- Automated red cell exchange (RCE), manual RCE, or simple transfusions suggested in patients with SCD and moderate acute chest syndrome:
- There is insufficient evidence to support automated RCE or manual RCE over simple transfusions in patients with SCD and moderate ACS.
- Automated or manual RCE should be considered for patients with one or more of the following:
- With rapidly progressive ACS.
- Who do not respond to initial treatment with simple transfusion.
- High pretransfusion hemoglobin levels that preclude simple transfusion.
- Automated RCE or manual RCE suggested over simple transfusions in patients with SCD and severe acute chest syndrome:
- Automated RCE is preferred over manual RCE to more rapidly reduce HbS levels.
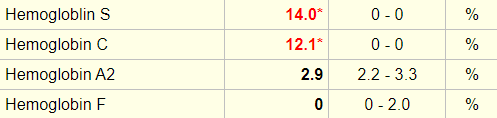
- A pre- and postprocedure complete blood count and hemoglobin fractionation should be obtained to maximize procedure safety and efficacy.
Which of the following are advantages of exchange transfusion over simple transfusion:
Transfusion recommendations depend on severity of acute chest syndrome.
There are no specific markers of disease severity but the following may be considered indicative of severe disease:
- A significant decline in the hemoglobin concentration.
- A significant decline in oxygen saturations (SpO2 < 95% or several percentage points below the patient’s baseline).
- Increasing respiratory distress.
- Progressive pulmonary infiltrates.
Here is a reminder of the patient’s presenting complete blood count:
| Day | WBC (109/L) | Hb (g/dL) | MCV (fL) | PLT (109/L) |
|---|---|---|---|---|
| Day of transfer | 15.4 | 6.9 | 75 | 92 |
| 6 months prior | 8.1 | 12.3 | 73 | 155 |
Here is a reminder of the patient’s presenting complete blood count:
| Day | WBC (109/L) | Hb (g/dL) | MCV (fL) | PLT (109/L) |
|---|---|---|---|---|
| Day of transfer | 15.4 | 6.9 | 75 | 92 |
| 6 months prior | 8.1 | 12.3 | 73 | 155 |
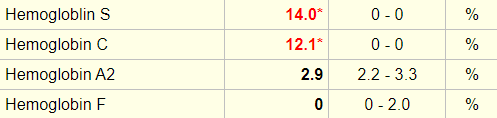
He had a Hb electrophoresis performed on the day following admission. These are the results:
This patient was admitted to the medical intensive care unit and was treated as follows:
- Exchange transfusion x 1 on first day
- Pain management with opioids
- Supplemental oxygen
- Incentive spirometry
Her arterial oxygen saturation improved, his CXR cleared and she was discharged 5 days after admission.
The discharge note commented on the following issues:
- Acute chest syndrome – resolved following treatment as outlined above; discharge oxygen saturation on room air 94%-98%
- Pneumonia:
- Initially started on azithromycin and ceftriaxone.
- Coverage then broadened with vancomycin, ceftazidime and azithromycin.
- Transitioned to oral Cefpodoxime to continue as an outpatient.
- Thrombocytopenia – resolved
The patient was advised to start hydroxyurea, but she declined.

