Treatment
Prev
1 / 0 Next
Prev
1 / 0 Next

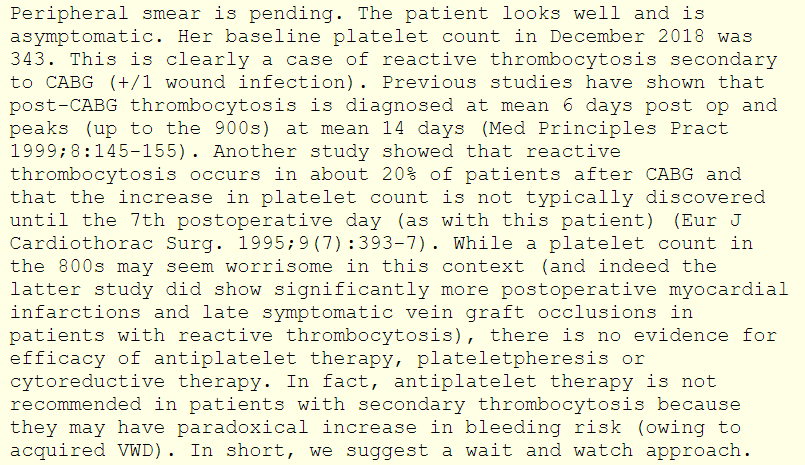
The cardiovascular surgery team claims that the patient’s current platelet count renders her at high risk for occluding her graft or developing a stroke. They are pressuring you to treat the patient with an anti-platelet agent or an anticoagulant. In addition to treating the underlying infection, what would you recommend?
a
Aspirin 81 mg daily
b
Therapeutic heparin
c
Hydroxyurea
d
Plateletpheresis
e
No intervention
There is some weak evidence that thrombocytosis in the postoperative period may be associated with higher rates of vein graft occlusion, but there is no evidence that treating with anti-platelet agents or cytoreductive therapy is helpful in this setting.
The following is an excerpt from the hematology consultation note:
The patient’s platelet count decreased over the next several days reaching normal levels 8 days later. She was discharged home with a normal complete blood count.
Prev
1 / 0 Next
