Preparing to see the patient
Can we all agree that a Hct of 69.3 is very high?!
What should be going through your head as you prepare to see the patient?
Can we all agree that a Hct of 69.3 is very high?!
What should be going through your head as you prepare to see the patient?
- Is the patient experiencing symptoms of hyperviscosity?
- Is the patient at risk for thrombosis and/or bleeding?
- What is causing such a high Hct?
- What diagnostic tests are needed?
- What are the treatment options?
Let’s begin with some physiological principles.
In the following slides we will:
- Define viscosity.
- Consider the determinants of blood viscosity (hematocrit being the most important).
- Assess how blood viscosity affects blood flow.
Definition of viscosity
Viscosity can be defined as the resistance of fluids against flow, which is related to the internal friction of adjacent fluid layers sliding past one another. Fluids in the center of the tube (e.g., blood vessel) move at a higher velocity than fluids that abut the edge of the tube (e.g., endothelium) where drag occurs.
(Think of viscosity as the “thickness” or “stickiness” of a fluid.)
Learn more here.
Parameters that determine blood viscosity
- Concentration and deformability of cells:
- Red blood cells (RBCs):
- Important parameters include:
- Hematocrit (Hct) :
- The most important determinant of blood viscosity under normal conditions.
- Impact on blood viscosity is much higher at low shear rates (e.g., in veins) than at high shear rate (e.g., in arteries).
- RBC deformability:
- Depends on:
- Internal (cytosolic) viscosity, mainly determined by the mean cell hemoglobin concentration.
- Membrane viscoelasticity, which is dependent on cytoskeleton proteins and lipid bilayer properties.
- Surface-area-to-volume ratio.
- Depends on:
- Hematocrit (Hct) :
- Important parameters include:
- White cells
- Platelets
- Red blood cells (RBCs):
- Concentration of plasma proteins:
- Fibrinogen
- α1-globulins
- α2-globulins
- β-globulins
- γ-globulins
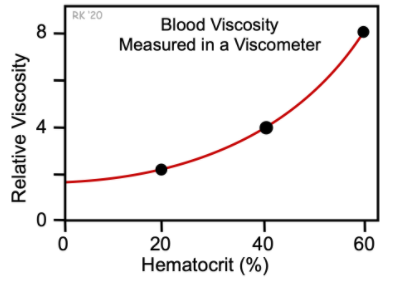
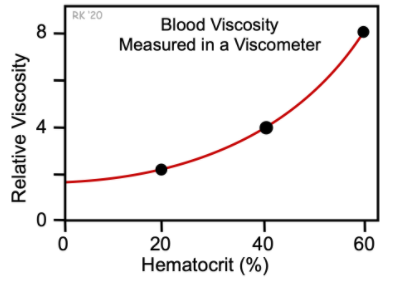
Of all the parameters above, the Hct is the most important determinant of blood viscosity.
Blood viscosity as a function of the hematocrit:
How blood viscosity affects blood flow
Poiseuille’s Law predicts that any increase in blood viscosity should cause a rise in vascular resistance.
Flow velocity in a given tube depends on pressure and flow resistance. According to Poiseuille’s Law, flow resistance depends on the geometry of the tube [length (l) and radius of the tube (r)] and the fluid’s viscosity (η). Flow velocity is calculated using the following formula:
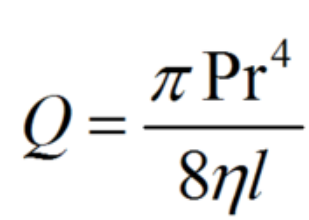
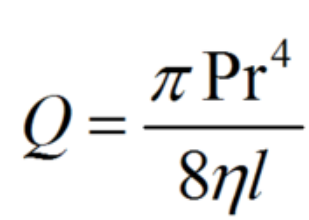
When applying Poiseuille’s Law to the cardiovascular system, one must consider the mean arterial pressure, the radius and the length of the vessels, and the viscosity of the blood.
Notes:
- Whole blood is a non-Newtonian fluid, which means that its viscosity depends on shear rate. At low shear, blood cells aggregate, which induces a sharp increase in viscosity, whereas at higher shear blood cells disaggregate, deform and align in the direction of flow.
- The highest viscosity is in the postvenule system. Viscosity is actually lower in the capillary due to central streaming of deformable red blood cells.
Let’s rearrange Poiseuille’s Law into a formula that is more familiar to you and more relevant at the bedside.
We will make the following changes:
- Replace blood flow (Q) with cardiac output
- Replace pressure (P) with the mean arterial pressure
- Replace what’s left of the right hand side of the formula (πr4/8ηl) with 1/total peripheral resistance
Now we can rewrite the equation:
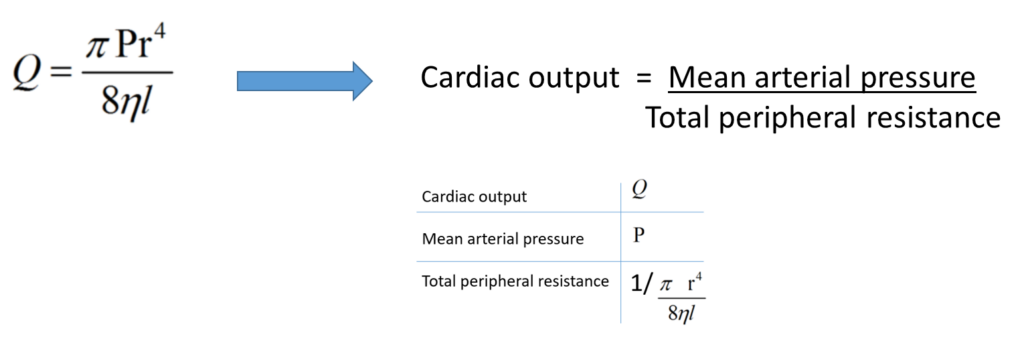
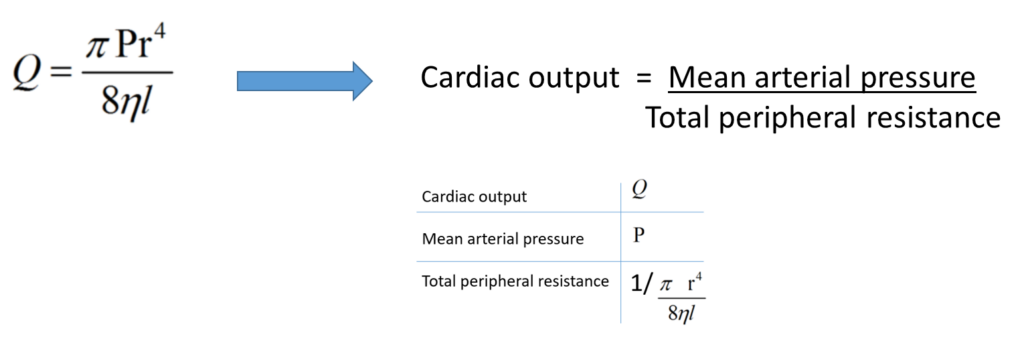
This way, we can appreciate that an increase in blood viscosity results in increased total peripheral resistance and decreased cardiac output.
In summary, an increase in Hct results in increased blood viscosity, which in turn increases total peripheral resistance and decreases cardiac output.
What are other causes of hyperviscosity?
Hypergammaglobulinemia is the most common cause of hyperviscosity syndrome. This is an example of elevated plasma viscosity.
Sometimes, the term plasma hyperviscosity is used to describe those cases attributed to increased concentration of plasma macromolecules, especially in monoclonal and polyclonal disorders associated with elevation of immunoglobulins.
Syndromes of high viscosity:
Mucosal hemorrhage:
- Epistaxis
- Gingival
- Gastrointestinal
- Retinal
Visual Disturbances:
- Retinal hemorrhage or thrombosis
- Papilledema
- Blurring
Neurologic:
- Somnolence or coma
- Cerebral hemorrhage
- Seizure
- Ataxia
Cardiac:
- High-output heart failure
Now you are armed with important background information as you prepare to see the patient.

